Dizzy? Tired? Anxious? You could have POTS
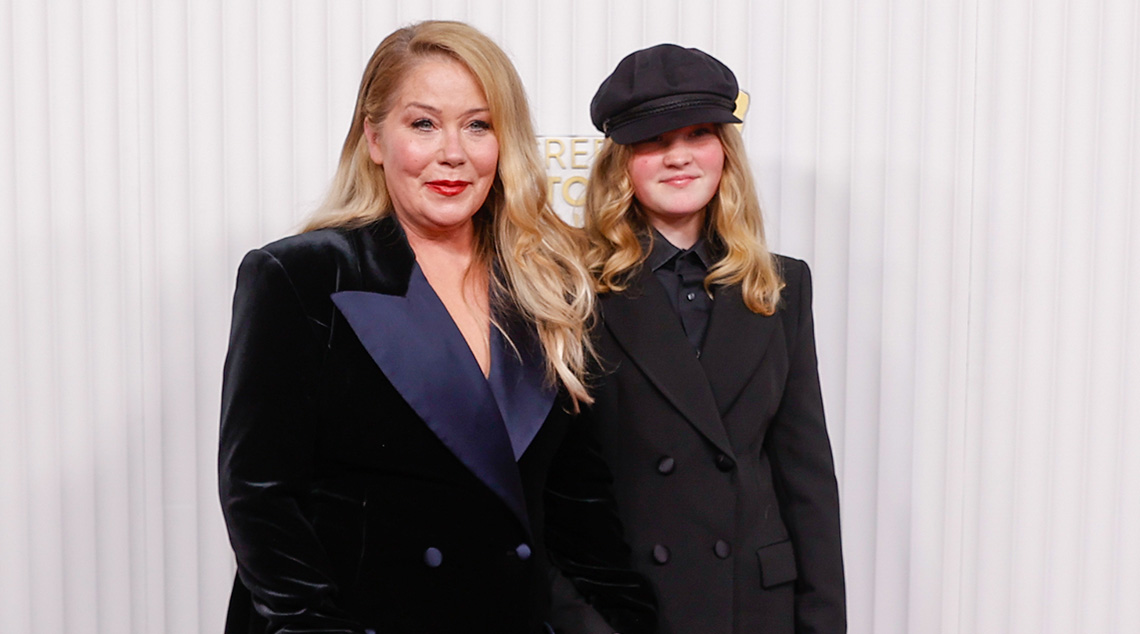
Actor Christina Applegate recently opened up about her daughter’s diagnosis with POTS. Here’s what you should know about the dizzying disorder.
Christina Applegate’s daughter, Sadie Grace LeNoble, was diagnosed with POTS a few months ago but only recently revealed her disorder on her mother’s podcast.
“I have something called POTS – postural orthostatic tachycardia syndrome,” Sadie, 13, said on the June 25 episode of the MeSsy with Christina Applegate and Jamie-Lynn Sigler podcast.
“It affects my heart and so when I stand up, I get really, really dizzy, and my legs get really weak, and I feel like I’m going to pass out,” she says.
“I have fainted before, and I have gone unconscious.”
Sadie said dealing with POTS had helped her empathise with her mother’s symptoms of multiple sclerosis, with which she was diagnosed in 2021.
Although Sadie’s diagnosis is recent, she says she has been dealing with the symptoms of her condition for a “long time”, revealing she was often dismissed by staff members at her school who thought she was lying about being sick to get out of class.
“They wouldn’t do anything for it and that definitely was hard,” she says.
General physician Dr Edmund Song says this is a common story among his patients.
“There are stories of people having their symptoms ignored or dismissed for years and years before their formal diagnosis,” he says.
What is POTS?
POTS, or postural orthostatic tachycardia syndrome, primarily affects the regulation of blood flow and volume, resulting in an abnormal increase in heart rate when a person moves from lying down to standing up.
Anyone can be diagnosed with POTS, but teenagers and adults between 15 and 50 are more likely to experience symptoms of POTS.
“There is a small subset of men that have POTS, but most are typically women,” Dr Song says.
Evolving Pain occupational therapist Amy Gowland explains that teenagers and young women are particularly susceptible due to factors such as “long COVID, chronic fatigue conditions, and connective tissue disorders such as hypermobility”.
According to the Australian POTS Foundation, it is not always clear what causes POTS, however, certain events or conditions can trigger symptoms.
- Infections and viral illnesses: POTS may develop following an infection or viral illness, such as Covid-19 or glandular fever.
- Surgery and trauma: POTS can also be triggered by surgery or traumatic events, including concussions.
- Hormonal changes: Hormonal fluctuations during significant life events such as pregnancy, menopause, or puberty can sometimes trigger POTS symptoms.
- Connective tissue disorders: Individuals with hypermobile Ehlers-Danlos syndrome (hEDS), a connective tissue disorder, are at an increased risk of developing POTS.
This condition can cause a wide range of symptoms, making everyday activities challenging for those affected.
“POTS affects the entire autonomic nervous system, impacting many involuntary functions and putting the body into a constant fight-or-flight response,” Ms Gowland says.
What are the symptoms of POTS?
Common signs and symptoms can include:
- Dizziness or light-headedness
- Fainting or almost fainting
- Blurry vision
- Tingling or numbness
- Noticeable heartbeats (heart palpitations)
- Chest pain
- Difficulty focusing
- Bloating
- Feeling too hot or too cold
- Headaches
- Tiredness
- Shortness of breath
- Shaking and sweating
- Feeling anxious
Some people might only have mild symptoms that they can manage easily, while others might have more serious symptoms that make everyday life harder.
Dr Song says that sensory overload caused by POTS can make people diagnosed avoid daily activities.
“Standing in a queue at supermarkets is really overwhelming for people with POTS,” he says.
“POTS patients often have a physical anxiety associated with the sensation of being upright.”
How is POTS diagnosed?
Dr Song says the “golden standard” for diagnosing POTS is the tilt table test.
This involves the patient lying on their back strapped to a motorised table in a horizontal position for five or so minutes.
The table is then moved so the patient is almost vertical, where they remain for five to 45 minutes depending on signs of symptoms.
During the test, heart rate and blood pressure are monitored in each position.
“We often use a simpler test called the ‘poor man’s tilt table test’,” Dr Song says.
“This involves measuring blood pressure and heart rate while lying down and then standing up, to see if there’s a significant increase in heart rate and symptoms.”
What is the treatment for POTS?
Dr Song says although there is no cure for POTS, it is a condition that can be managed through lifestyle changes.
“Increasing fluid and salt intake to maintain blood volume is important.
“Exercise, especially targeted leg exercises and aerobic activities, can also help manage symptoms by improving cardiovascular efficiency,” he says.
“Many patients can lead normal lives with lifestyle interventions and sometimes medications, but there’s always a tendency for symptoms to recur, especially during times of stress or illness.”
Ms Gowland adds that compression garments are another option to help improve blood flow regulation.
“It is highly recommended for POTS clients to use compression garments that go over the stomach and down to the ankles,” she says.
“Patients tend to have blue- or purple-coloured legs due to low blood circulation. So, these garments help to promote blood flow back up to the brain.”
Mr Gowland says if you think you have POTS, don’t be afraid to seek help from a GP, medical specialist or allied health practitioner.
“It’s crucial to ask questions and advocate for yourself because the impact on daily function can be significant.”
More on health:
- What you need to know about Ehlers-Danlos syndrome
- In a spin? What you should know about vertigo
- Could lupus be causing your health problems?
- Everything you need to know about multiple sclerosis
Written by Sarah Varcoe.